Type IV hypersensitivity is also known as delayed-type hypersensitivity. Because this hypersensitivity reaction takes more than 12 hours to develop whereas the typical maximum reaction time is 48 – 72 hours. It is a cell-mediated type immune response. It involves T cells that are responsible for inflammatory reactions in response to either exogenous antigens or autoantigens. Usually, these types of hypersensitivity reactions to exogenous antigens involve other antigen-presenting cells (APC) such as macrophages also.
Generally, CD4+ Th1 helper T cells recognize APC with a foreign antigen complex with the Major Histocompatibility Complex (MHC) Class II on the surface. It then triggers these reactions. Macrophages that secrete cytokine IL-12 stimulates the proliferation of CD4+ Th1 cells. These cells are capable of secreting cytokines IL-2 and interferon-gamma (IFN-γ) which in turn mediates the release of Th1 Cytokines. Together they perform the immune response against the antigens. Activated CD8+ T cells in the process destroy the APC and activate macrophages to release hydrolytic enzymes. Once these reactions go beyond the norm they damage internal tissues, cause unnecessary inflammations, and cell death.
Tubercular Lesions
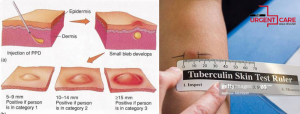
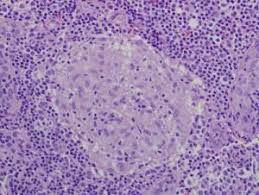
Tubercular lesions come under Type IV hypersensitivity as a form of granulomas. Tuberculin is a protein derivative that is used to diagnose tuberculosis. The immune system recognizes attenuated M. tuberculosis cells in tuberculin as foreign bodies. Then with the collaboration of macrophages, it attacks the APC. However, as a result of the immune-escape mechanism processed by mycobacteria, at first, bacterial cells can avoid being destroyed. Eventually, macrophages become hyperactivated and recruit multiple monocytes, resulting in significant inflammation, local damage, and granulomas.
A granuloma forms during an inflammation, from the macrophages, when they try to wall off a foreign APC and ultimately fail. It is a significant feature, whether the granuloma contains necrosis or not, referring to dead cells appearing as a nucleus-less mass of cell debris. It is known as caseation.

Graft Rejection
The same kind of process and consequences are related to graft/transplant rejections which makes them also Type IV hypersensitivity. Transplantation is the process of moving cells, tissues, or organs from one site to another to replace or recover damaged or diseased sites. Yet the immune system presents many obstacles when transferring body parts from a donor to a recipient unless they are identical twins.
The immune system, under normal situations, works to identify and destroy foreign pathogens. Thus if it recognizes the transplant as foreign, launches a rejection reaction. This might result in destroying the transplant.
Types of Transplants
There are 3 types of transplants;
- Autograft – Transplanting tissues or organs between different body sites of the same individual.
- Allograft – Transplanting tissues or organs between a donor and a genetically non-identical recipient. If the donor and recipient are identical twins, then the graft is said to be ‘Isograft’
- Xenograft – Transplanting tissues or organs between individuals of two different species.
Allografts are the main subject for immunological graft rejection. Rejection is a reaction involving both cell-mediated and antibody-mediated hypersensitivity reactions against major histocompatibility complex (MHC) containing cells on the foreign graft. Thus it is of vital importance to find the most eligible donor-recipient match during a transplant. In addition, immunosuppressive drugs are often used to prevent graft rejections.
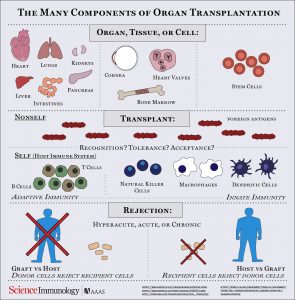
Types of Graft Rejections
These rejections can be of 3 types;
- Hyper-acute rejection – occurs within hours of transplantation due to pre-existing antibodies within the recipient.
- Acute rejection – occurs within 6 months of transplantation caused due to the formation of antibodies as a result of identifying foreign antigens within the donated graft.
- Chronic rejection – continuous acute rejection finally resulting in complete rejection and failure of the transplant.
Alloimmunity refers to an immune reaction triggered by an alloantigen. It can processes antigens in 2 ways as; Direct recognition of non-self Human Leucocyte Antigen (HLA) which are MHC Class II antigens expressed in donor Antigen Presenting Cells (APC) from transplant and the Indirect recognition of alloantigen derived peptide self-HLA which are MHC Class I antigens. Once sensitized they develop antibodies and cell-mediated responses.
Phases of Graft Rejection
First T cell receptors recognize donor HLA antigens on the recipient allocative T lymphocytes. As a result, they stimulate a cascade of reactions which finally leads to graft rejection. Rejection happens in 2 main phases;
- Sensitization phase – the proliferation of antigen reactive lymphocytes in the recipient’s lymph nodes
- Effector phase – the destruction of graft by sensitized cells.
During initial sensitization proliferation of CD4+ and CD8+ T cells take place in response to alloantigens. Interaction of CD4+ T cells with an APC carrying proper peptide-HLA complex within dendritic cells and vascular endothelial cells activates the T cells for vigorous proliferation. CD4+ being the main proliferating cells, directly identify HLA class II antigens.
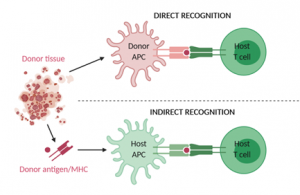
These reactions result in 2 potential graft rejection mechanisms. One is a direct recognition of the graft which requires the presence of APCs in the graft and enough lymphatic drainage to regional lymph nodes. Second is the indirect recognition of the graft where the recipient’s APCs take up foreign proteins released from the graft resulting from a pro-inflammatory environment.
Apart from the above reactions, complement-dependent antibody lysis or natural killer (NK) cell destruction by antibody-dependent cell-mediated cytotoxicity (ADCC) can also take place. Recognition of donor’s HLA class I antigens by CD8+ cells drives Cytotoxic T Lymphocyte or CTL-mediated killing of graft cells. CD4+ cells function as HLA class II cytotoxic cells.
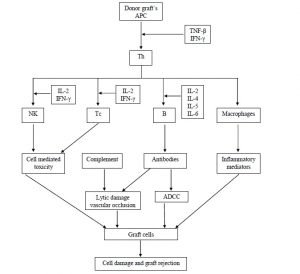
During effector mechanisms, cytokines such as IL-2, IFN-γ, and TNF-β play important roles. IL-2 stimulates T cell proliferation and helps the generation of effector CTLs. IFN-γ induces Th1 responses and with TNF-β stimulate macrophage influx.
With the advancement of technology and owing to immunological researches, transplant medicine has improved drastically. However, immune rejection of grafts remains a formidable barrier for a successful transplant.
References :
- Justiz Vaillant AA, Zulfiqar H, Ramphul K. Delayed Hypersensitivity Reactions. [Updated 2020 Jul 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519023/
- Kumar, Vinay., Abbas, Abul K., Aster, Jon C.Robbins, Stanley L. (Eds.) (2013) Robbins basic pathology /Philadelphia, PA: Elsevier/Saunders
- Deathridge, J., 2020. Transplant Immunology. [Online]
Available at: https://www.immunology.org/policy-and-public-affairs/briefings-and-position-statements/transplant-immunology
Image Courtesy :
- Title image: https://bit.ly/3f0s1E3
- 1st Content image: https://bit.ly/3nXkpGt
- 2nd Content image: https://bit.ly/3xWHi1y
- 3rd Content image: https://bit.ly/3hbEwzA
- 4th Content image: https://bit.ly/2RAHrH2
- 5th Content image: http://t.ly/VnbO